 Have you heard? There’s a Pelvic Floor Disorder Pandemic!
Have you heard? There’s a Pelvic Floor Disorder Pandemic!
It’s not an infectious disease, but it is rampant and worldwide, and increasing in numbers.
I was shocked when I first started working with uterine and pelvic issues, to meet young women—in their 30’s—with their uterus hanging outside their body, between their legs, because it had prolapsed after giving birth.
Until then, I also didn’t realize how many women of all ages experience intermittent dribbling of urine, or stress incontinence, and wore pads because of it.
I didn’t know the numbers of women who were having painful sex or no sex at all because of pain and birth trauma— for years after giving birth.
I didn’t realize how many women described their birthing experience as traumatic, even when it classified as a ‘normal’ birth, and found that trauma residing in their pelvic floor muscles.
I found this all out because these people were coming to see me for pelvic floor bodywork, hoping I could help them. After seeing these conditions for some time, I started to learn that about 1/4 of ALL adult women in the USA over 20 years old, and at least HALF of women over age 80, suffer from pelvic floor disorders (PFD) That’s alot of women, isn’t it?! MIllions! This should be acknowledged as an epidemic!! Globally the rate of PFD is just as high or likely even higher.
IT REALLY IS A PANDEMIC!
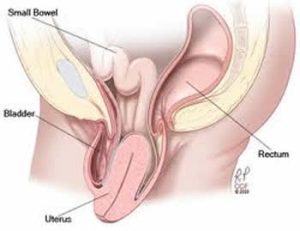 On the other hand, up to 400,000 American women annually are impacted so severely with PFD that they do see someone, and end up having surgery --mostly for incontinence and prolapse--to try to improve the condition. A large number of these are their second or third surgery for that issue!
On the other hand, up to 400,000 American women annually are impacted so severely with PFD that they do see someone, and end up having surgery --mostly for incontinence and prolapse--to try to improve the condition. A large number of these are their second or third surgery for that issue!
Some find surgery to be beneficial, but it is not always successful—One study found a 60-70% failure rate for prolapse surgery!! (Yes.. that’s FAILURE rate!—meaning the prolapse returned within 5 years post-surgery!)<Duke Clinical Research Institute 4-17-18. https://dcri.org/prolapse-surgeries/>). Meanwhile, surgery creates scar tissue, and scar tissue often causes more pain, restrictions and problems than the reason for the surgery in the first place!

Pelvic Floor Disorders (PFD) Stats
- 1 in 5 women (and some studies say 1 in 3) after age 20 have PFD
- Nearly half of all women over age 80 have PFD
- Surgery for prolapsed organs is expected to increase 48.2% in the next 30 years
Despite these harrowing statistics, Pelvic Floor Disorder has not actually been classified as an epidemic or a pandemic. Why not?! It doesn’t have to be an infectious disease to be classified that way. Obesity is considered an epidemic. Why not PFD?
Could it correlate with the fact that...
- it is mostly women who experience it
- it occurs in a zone that’s taboo to talk about or and less likely to be explored than the Moon
- it’s a place many feel ashamed of?
Discomfort and dysfunction in a woman’s “down there” zone is a deep, invisible secret, literally hidden away. Unless you tell somebody, no one will ever know you have it. And yet it occupies a vast amount of attention in the minds of those who suffer.
What if you could be relieved of the problem with skilled bodywork?
- What if skilled touch and attention to pelvic muscles could help them remember that they have the power to work in a unified manner to reduce incontinence.
- What if releasing long-held tension from surgery, birth, emotional tension, or abuse created more blood flow and optimized pelvic health?
- What if postural awareness shifted the pressure on the uterus so it did not prolapse so far?
Would that be worth talking about it then?
This doesn’t have to be a secret!! Secrets gain strength and power from the energy it takes keep it hidden. They breed shame or anxiety. By naming the secret, by bringing it out of the shadows to be seen, it begins to dissolve and the power it has stolen can be recovered to its rightful owner.
By the way—What is a Pelvic Floor Disorder (PFD) exactly? 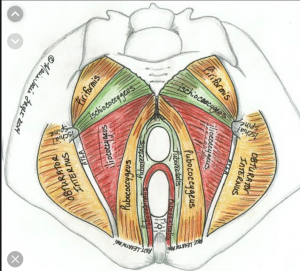
Watch for that blog post! But for now, suffice to say this:
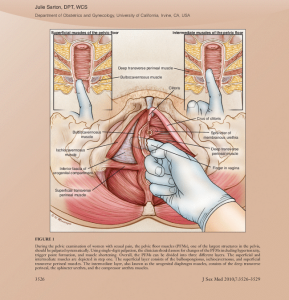
The pelvic support system, like the rest of the musculo-skeletal system, is made up of muscles, ligaments, and nerves woven together in complex arrangement that supports, engages, invites, releases, and mobilizes. Generally, when tissues, ligaments, muscles, bones are stretched, injured, weakened, and become imbalanced or misaligned, they can’t function properly, to do the job they are intended to do. In this case, pelvic muscles are designed to support posture and pelvic organs, align with the movement of the respiratory diaphragm, control the release of urine and stool, and relax and open for sexual experiences and birthing. The vast majority of women with PFD develop issues after giving birth, (although birthers are not the only ones who suffer problems!). Other reasons are listed below in the box:
SO what to do?
Looking at the big picture, it’s not too hard to see why this so prevalent around the world. Not only is women’s health overall less funded, less researched, less focused on than men’s health, but societal sexual practices, birth practices, work stressors, and body mechanics, can all create pelvic tension and impact these muscles that are integral to our spinal/physical support. Not to mention rampant sexual abuse in a society that does not make space for women’s sexuality and fertility cycling.
It’s a big bowl of issues and the “why” is a BIG story for another time. Basically, we need to develop strong healing practices that can support full body health in a challenging world, and support pelvic floor muscles to work properly and be in balance with one another so they can comfortably engage And relax.
Common Reasons for Developing PFD
- Menopause
- Hysterectomy
- Vaginal birth with long pushing, or use of vacuum extractors or forceps
- Lack of postnatal recovery support
- Obesity or other reasons for increased abdominal pressure
- Smoking or Connective tissue disorders.
- Living in societies embedded with rampant sexual abuse
- 2000 years of patriarchal dominion over women’s bodies & cycles
It’s not just people with incontinence or prolapse who benefit from this work. 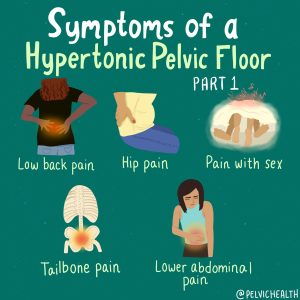 Pelvic Floor Bodywork is useful for anyone who gave birth—an experience that seriously alters the pelvic muscles! Anyone who has had pelvic/hip/back injuries, abdominal surgeries, or even knee/foot/leg problems can find symptoms improve with this work. (Yes—the foot is connected to the pelvic floor!)
Pelvic Floor Bodywork is useful for anyone who gave birth—an experience that seriously alters the pelvic muscles! Anyone who has had pelvic/hip/back injuries, abdominal surgeries, or even knee/foot/leg problems can find symptoms improve with this work. (Yes—the foot is connected to the pelvic floor!)
I’ve worked with super-yogis who have practiced so many pelvic floor contractions without understanding the importance of relaxing the muscles as well, that they have ended up with hypertonic muscles causing various pains and birthing challenges. Bodywork should be tried first before moving toward surgery and it can be helpful for healing the body and mind after surgery. It can’t provide total relief for Everyone, but it certainly can provide some relief for many, and full relief for lots. It is an opportunity for Self-Healing—when supported to revision one’s relationship to this sacred zone. It can be enlightening. It causes no problems. And it’s way more comfortable than surgery!
Integrative Pelvic Bodywork
 My form of Integrative Pelvic Bodywork weaves together this internal bodywork with external bodywork, and awareness and attention to the mind/spirit/emotional body that is entirely entwined with physical form. Healing is possible using sensitive, skilled muscle-bone-ligament-nerve bodywork that helps restore normal pelvic floor function.
My form of Integrative Pelvic Bodywork weaves together this internal bodywork with external bodywork, and awareness and attention to the mind/spirit/emotional body that is entirely entwined with physical form. Healing is possible using sensitive, skilled muscle-bone-ligament-nerve bodywork that helps restore normal pelvic floor function.
While Physical therapists are the primary professionals who do internal pelvic bodywork, Massage therapists can do it also in Oregon and a few other states.

What's the difference between Physical Therapist vs Massage Therapist Pelvic Bodywork?
We usually offer something different than a PT. These are generalizations, but based on my own and my client’s experiences and descriptions:
- Generally we are less clinical, and spend more time with a client than a PT can. Typically a massage therapist’s office is more relaxing and inviting for healing the whole, rather than typical PT office.
- Like PT’s, we may help address postural issues contributing to PFDs as well. This is important because the patterns of holding and stress that become our posture, or develop from our posture, will impact the position of the womb and the pelvis, and the quality of energy flowing through this area of the body.
- Massage therapists may hold space for potential somatic-emotional release of traumatic energy caught in this potent creative root center.
- Massage therapists usually also provide massage to the head and neck and jaw to help move the energy that released from below, upward, and overall relaxing “comfort touch”.
- Massage therapists can release energy in a client’s hands and feet to provide grounding and rebalance pelvic misalignments with external muscular release.
- A patriarchal and religious suppression of feminine energies has dominated the world for 2000 years—creating a big underlying wound embedded in most pelvises—Including Male pelvises! Patriarchy has negative impacts on All people, and Benefits a few.
- More on that in another blog post to come: The Yoniverse vs The Patriarchy
In the upcoming blog posts I’ll be talking more about the issues and possibilities to resolve them, and the applications of Integrative Pelvic Bodywork.
 WANT TO LEARN MORE?!
WANT TO LEARN MORE?!
Join the upcoming class for bodyworkers & health professionals: Entering the Temple: Bodywork for the Female Pelvic Floor.
REFERENCES
- Dieter AA, Wilkins MF, Wu JM. Epidemiological trends and future care needs for pelvic floor disorders. Curr Opin Obstet Gynecol. 2015 Oct;27(5):380-4.
- Hallock JL, Handa VL. The Epidemiology of Pelvic Floor Disorders and Childbirth: An Update. Obstet Gynecol Clin North Am. 2016 Mar;43(1):1-13.
- Kenne, K.A., Wendt, L. & Brooks Jackson, J. Prevalence of pelvic floor disorders in adult women being seen in a primary care setting and associated risk factors. Sci Rep 12, 9878 (2022).
- Nygaard I, Barber MD. Prevalence of Symptomatic Pelvic Floor Disorders in US Women. JAMA. 2008;300(11):1311–1316.
"Out of 25,425 adult women attending primary care clinics, one study in 2008 found that 32.0% of the women had at least 1 PFD. Bowel dysfunction the most common (24.6%), followed by urinary incontinence (11.1%) and Pelvic Organ Prolapse (4.4%).Nygaard et al. found that approximately one quarter of women in the United States have at least 1 PFD..." - Smith FJ, Holman CDJ, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstetrics & Gynecology. 2010;116(5):1096–1100.
- Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime Risk of Stress Urinary Incontinence or Pelvic Organ Prolapse Surgery. Obstetrics & Gynecology. 2014;123(6):1201–1206.
- https://www.healthyagingpoll.org/reports-more/report/urinary-incontinence-inevitable-part-aging
- https://www.memorialhermann.org/services/specialties/pelvic-floor/pelvic-floor-disorders
: